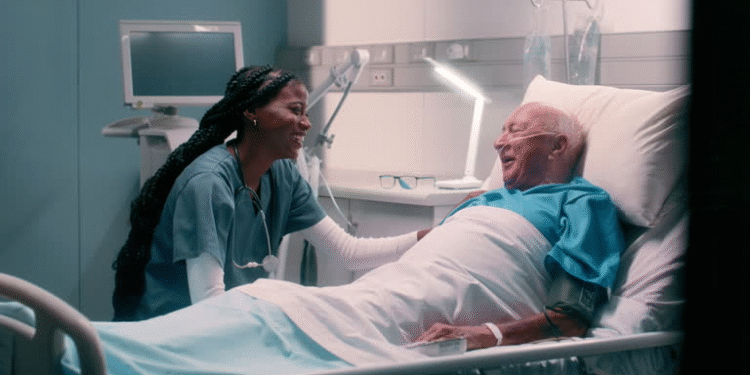
In a field where time is short, resources are stretched, and the stakes are incredibly high, measuring performance is essential. But when it comes to healthcare, productivity isn’t just about numbers it’s about outcomes, quality, and the patient experience. That’s why productivity metrics in healthcare are both necessary and complex.
Unlike traditional industries where output is easily quantifiable, healthcare involves nuance. You’re not just counting units or hours you’re evaluating the effectiveness of care, provider workload, efficiency, and overall system performance.
Why Productivity Metrics in Healthcare Are Unique
Productivity in most sectors is a straightforward equation: input vs. output. But in healthcare, this calculation gets complicated. A physician who sees 40 patients a day might seem highly productive, but what if half of those visits are rushed or lead to misdiagnoses? On the flip side, a clinician who takes more time per patient might produce better outcomes, but appear less efficient on paper.
That’s the challenge with measuring productivity in healthcare it’s not just about volume. It’s about value.
Productivity metrics in healthcare need to balance quantity and quality. They should reflect how well providers are delivering care, using time, and managing resources without compromising the human side of medicine.
Common Productivity Metrics in Healthcare
Healthcare systems use a range of metrics to evaluate productivity. Some are quantitative, others qualitative. Each tells part of the story.
1. Work Relative Value Units (wRVUs)
One of the most widely used benchmarks, wRVUs measure the value of services based on time, skill, and complexity. They’re used to compare provider output and standardize performance.
2. Patient Encounters Per Day
This metric tracks how many patients a provider sees in a given day or week. While useful, it can be misleading if not considered alongside quality indicators.
3. Length of Stay (LOS)
In inpatient settings, reducing average LOS without compromising care is seen as a marker of efficiency and good case management.
4. No-Show and Cancellation Rates
These reflect how effectively an organization is managing its schedule and patient communication. High rates may indicate system or access issues.
5. Chart Completion and Documentation Timeliness
Timely, complete documentation is critical not just for billing, but also for continuity of care and compliance.
6. Patient Satisfaction Scores
Though subjective, patient feedback provides context to productivity metrics. A high-volume provider with low satisfaction scores may raise red flags.
The Importance of Tracking Productivity Metrics
Productivity metrics in healthcare serve several essential functions:
1. Resource Allocation
Hospitals and practices need to know where time and money are going. Are certain departments overwhelmed while others are underutilized? Are providers managing their caseloads efficiently? Metrics help decision-makers allocate support where it’s needed most.
2. Performance Improvement
Tracking metrics allows clinicians to self-assess and improve. It provides feedback on what’s working and what needs adjustment. For instance, if a provider has high patient volumes but poor follow-up rates, that insight can spark targeted training or workflow changes.
3. Compensation and Incentives
Many organizations link compensation to productivity especially when using wRVUs or similar benchmarks. While this can drive motivation, it must be balanced with quality measures to avoid encouraging quantity over care.
4. Compliance and Risk Management
Proper documentation and billing aren’t just financial necessities they’re legal requirements. Metrics help ensure staff are meeting these obligations and help catch issues before they become problems.
5. Operational Efficiency
Metrics show where time is being lost. Are providers spending too much time charting? Is appointment scheduling inefficient? Are follow-up calls delayed? Productivity data highlights friction points that can be streamlined.
Challenges of Using Productivity Metrics in Healthcare
Despite their value, metrics are not without pitfalls. Here are some of the challenges:
- Oversimplification: Reducing complex clinical work to numbers can undervalue important but less quantifiable tasks like patient education or emotional support.
- Burnout Risk: Overemphasis on productivity can pressure providers to rush care or work longer hours, leading to burnout.
- Data Overload: Too many metrics or poorly chosen ones can distract rather than clarify.
- One-Size-Fits-All Approaches: Not all specialties or roles can be measured the same way. What works for a surgeon doesn’t apply to a social worker or care coordinator.
That’s why the best organizations use productivity metrics in healthcare as one piece of a bigger picture, pairing them with outcome measures, peer reviews, and contextual understanding.
Making Metrics Meaningful
So how do you use productivity metrics in healthcare without losing sight of the mission? Here are some guiding principles:
1. Measure What Matters
Focus on metrics that align with your organization’s goals and patient needs not just what’s easy to track.
2. Balance Quantity with Quality
Include clinical outcomes, patient satisfaction, and safety measures alongside productivity data to get a full picture of performance.
3. Give Providers Insight, Not Pressure
Use metrics as tools for self-awareness and improvement, not just as sticks to enforce quotas.
4. Adjust for Specialty and Context
Customize metrics for different departments, roles, and patient populations. Fairness improves buy-in.
5. Keep the Human Element in Focus
Remember that behind every data point is a person both the patient and the provider. Compassion and care should remain at the heart of healthcare, no matter what the numbers say.
Final Thoughts
Productivity metrics in healthcare are powerful tools when used thoughtfully. They help organizations run more efficiently, support better outcomes, and empower providers to grow. But they work best when paired with empathy, context, and a genuine commitment to high-quality care.
As healthcare continues to evolve, measuring productivity will remain essential but so will remembering why we measure it in the first place: to help people, not just count them.